Parenting Issues
 for Women with Co-Occurring Mental Health and Substance Abuse Disorders Who Have Histories of Trauma.
for Women with Co-Occurring Mental Health and Substance Abuse Disorders Who Have Histories of Trauma.
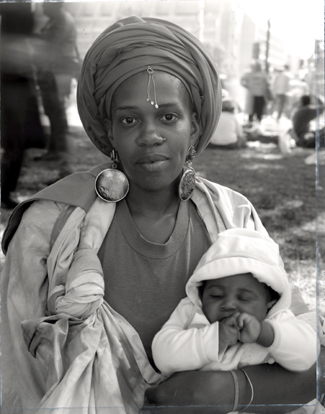
Many women with co-occurring mental health and substance abuse disorders and histories of trauma are parents who value their roles as mothers and bring
skills to the task.
Historically, treatment for these women has neither considered the importance of women’s roles as mothers nor included their children.
Treatment can be optimized by acknowledging their roles as parents and incorporating this reality into service design and delivery.
Many Women With Co-occurring
Conditions Are Parents
Millions of women in America suffer from cooccurring substance abuse and mental health
conditions.
1
A substantial majority of women with these co-existing conditions have also experienced violence.
Women who struggle to overcome these problems are likely to have more severe difficulties and use services more often than women with any one of these problems alone.
2
Because services tend to be fragmented, and treatment philosophies can be
inconsistent, these women face barriers to adequate care.
3
Chief among these barriers is the fact that many of these women are mothers caring for dependent children.
4
No comprehensive data have documented the number of women with co-occurring conditions and trauma who are mothers. Large-scale surveys do not
emphasize the role of motherhood and public health departments generally do not keep statistics on parenting rates.
5
One exception, a study of women using illicit substances in a large urban area,
demonstrated that 60% to 70% of respondents have children.
6
A number of these women do not have custody of their children, but their identities as mothers are still primary and many want to reunify with their children.
Most women with co-occurring conditions and trauma histories view parenting as the central purpose and defining role of their lives.
7
For them, motherhood is both a major source of identity and self worth, and a
source of shame and guilt.
8
Their “mothering” can be a primary motivation for entering treatment or a
deterrent to seeking care. In short, a woman’s identity as a mother, figures importantly into her self-esteem, behaviors, and treatment decisions.
“…true recovery for a mother usually
works only when it includes her
children.”
-Norma Finkelstein, Ph.D.
Parenting Is Not Generally Incorporated
Into Treatment
Although considerable attention has been given to
women’s treatment needs in the areas of mental
health, substance abuse,
9
trauma,
10
and co-occurring disorders,
11
current service models are largely based on women as individuals, rather than as parents. The few studies that have examined intergenerational
issues generally do so in the context of breaking the cycle of abuse.
12
Some researchers view this approach as outmoded; as expressed by Finkelstein, “The attitude that recovery must come first and that women need their own space to recover and cannot concentrate on their recovery with children present reflects a lack of understanding of access issues, of maternal and child health issues, and of the fact that true recovery for a mother usually works only when it includes her children.”
13
Co-Occurring
Women,
Disorders &
Study
Violence
Produced by the Coordinating Center of the SAMHSA
Women, Co-Occurring Disorders and Violence Study
Parenting Issues for Women with
Co-Occurring Mental Health and
Substance Abuse Disorders
Who Have Histories of Trauma
Despite the prevalence of motherhood in this population and the fact that programs providing parenting, child care, and children’s service attract more women,
14
very few programs include children in their mother’s treatment. The lack of services for mothers and children together acts as a major barrier to treatment. Many mothers do not enter treatment because they don’t want to lose their children.
15
A recent survey of 78 drug treatment programs in New York City found that 54% excluded pregnant women, and 67% would not treat pregnant Medicaid
patients.
16
Another survey of state mental health programs found that only four states have residential programs for mentally ill women and their children, and no state had a policy about a child visiting a hospitalized mentally ill mother.
Only half of the states had programs for assessing parenting skills and outpatient services to improve those skills.
17
Some programs that do admit children will terminate a mother if her child has behavioral problems, putting extraordinary pressure on the parent to monitor and control her child’s conduct.
To date, both the strengths and needs of pregnant and parenting women with co-occurring disorders and trauma have been largely overlooked. This is particularly ironic considering that the desire to keep or be reunited with their children is one of the strongest motivations for seeking assistance.
Co-occurring Conditions Can Influence
Parenting
Many women with co-occurring conditions and trauma histories have not had constructive preparation for parenting.18 Growing up in families with a
substance abusing or violent parent, or without consistent nurturing and discipline, they lack positive parenting role models.
Because of their experiences as children, they may feel ambivalent about their own children and unsure of their abilities as parents.
19
The nature of their complicated histories suggest that these women have needs for multidimensional supports and treatment modifications.
20
Adverse early life experiences and battles with mental illness, addiction, and trauma often result in high levels of distress which can impact parenting skills.
21
Research shows that women in this population may be at risk for problems in parenting or even for maltreating children.
22-25
Other significant contextual factors, such as poverty and homelessness, also
increase the likelihood for troubled interactions between parents and their children.
In addition, pregnancy and parenting may activate issues associated with a mother’s mental illness, substance abuse, or trauma. Psychiatric symptoms may intensify and warrant close monitoring.
26
Being pregnant or caring for a vulnerable child may activate feelings related to a trauma survivor’s own painful childhood. Among substance abusing mothers, a “treadmill phenomenon” may occur whereby guiltover using substances may prompt her to escalate her sage to escape these feelings..
27
Optimizing Treatment
Treatment for women with co-occurring conditions and histories of violence is optimized when it:
• Focuses on a woman’s strengths.
• Acknowledges a woman’s role as a parent.
• Improves interactions between the parent and
child.
• Provides comprehensive, coordinated services for
a mother and her children.
Focusing on Strengths
Dually diagnosed women with histories of trauma bring strengths to parenting that should be recognized and fostered. For example, most of these mothers are:
• Devoted to their children and strongly motivated to protect them.
• Compassionate and empathic toward children, who they may see as vulnerable to loss, grief, and hurt.
• Capable of enormous courage and perseverance. Programs and services should be based on women and children’s strengths rather than their deficits.
Acknowledging Women’s Roles as Parents Women’s roles as mothers should be acknowledged in all service delivery activities. From the initial assessment for pregnant or parenting women, questions should be asked about prior parenting
experiences, feelings about pregnancy and the fetus, expectations of the infant/child, and assessment of parent-child interactions.
28
Themes about mothering (e.g., being a role model to children, self-acceptance
for prior parenting behaviors, facing feelings related to parents in family-of-origin) should be interwoven into individual and group therapies. Treatment and
discharge planning should account for their role as parents. Hospitals and residential treatment facilities should ensure regular contact between a mother and her children.
29
Strengthening Parenting Skills Parenting skills can be improved through education and appropriate supports. Skill-building interventions may be most effective when they focus on parenting issues specific to women with co-occurring conditions and experiences of abuse.30 For example:
• Mothers may have inappropriate expectations for their children’s behavior. They can improve their parenting skills by becoming aware of their child’s developmental issues.
• Mothers may have lapses in empathy for children because they are absorbed with pressures in their own lives. When they are supported, mothers are able to pay better attention to their children’s needs.
• Mothers may engage in “role reversal,” causing them to look to their children for fulfillment of their own needs. Developing satisfying relationships with other adults may ease a mother’s need to turn to her children for sustenance.
• Some mothers espouse corporal punishment because they lack knowledge of alternatives.
Providing them with other strategies broadens their ability to mange their children’s behavior.
In addition, interventions that help to increase a mother’s “life skills” such as organizing and planning, coping with stress, problem-solving, and selfinstruction help to provide a consistent structure for positive interactions between mothers and their children.
31
Finally, for women with co-occurring conditions and trauma, attention should be paid to their struggle with debilitating levels of shame and guilt. Finkelstein emphasizes the importance of acknowledging these feelings: “Warranted or not, the guilt feelings are very real for them. If guilt is not allowed conscious
expression, it will almost certainly be misdirected…toward the family or against themselves in the form of depression, low self-esteem, or selfdestructive
behaviors.”
32
The Coalition on Addiction, Pregnancy, and Parenting in Cambridge, Massachusetts is one example of a successful demonstration project for substance abusing mothers.
33
The parenting component of this intervention includes 23 weeks of specialized individual and group services for both pregnant women and their children at long-term residential substance abuse treatment programs for women.
The three-part intervention includes: (1) a structured parenting skills group; (2) a child development group
providing specific information regarding children’s developmental stages; and (3) a Mothers’ Support Group where women share parenting experiences.
Women report dramatic increases in self-esteem, greater knowledge and frequent use of appropriate parenting techniques, and an overall sense of
improvement in parenting.
Providing Comprehensive, Coordinated Services
To effectively meet the needs of these women and their children, services must be comprehensive and coordinated. Specifically, a number of considerations should be incorporated into the design of all programs serving these women and their children.
34
These include the following:
• Issues of trauma, mental illness, and substance abuse should be interwoven in order to better
integrate services for these women. • Women’s concern that they will be reported to child protective services and/or lose custody of their children for seeking treatment must be explicitly addressed at the program and policy
levels.
• Services provided to mothers should not be predicated on their children’s behavior or conduct.
• Treatment should be responsive to the developmental needs of mothers and children. The needs of mothers with infants differ radically from those with preschool, school age, or adolescent children.
• Services should be family-centered, comprehensive, and multidisciplinary to ensure that the full-range of needs of both mother and child are addressed.
35
By including explicit parenting components as a part of the services that are available to women with cooccurring conditions and histories of violence, women can achieve positive outcomes that will also extend to their children. Thus, strengthening parenting skills and improving parent/child relationships holds wideranging implications for the health and mental health of the next generation.
1. Center on Addiction and Substance Abuse. (1996). Substance Abuse and the American Woman. NY: The National Center on Addiction and Substance Abuse at Columbia University.
2. Harris, M. (1994). Modifications in service delivery and clinical treatment for women who are diagnosed with severe mental illness who are also survivors of sexual abuse trauma. The Journal of Mental Health Administration, 21, 396-406.
3. Grella, C. E. (1996). Background and overview of mental health and substance abuse treatment systems: Meeting the needs of women who are pregnant or parenting. Journal of Psychoactive Drugs, 28(4), 319-343.
4. Harris, M. (1996). Treating sexual abuse trauma with dually diagnosed women. Community Mental Health Journal, 32, 371-385.
5. Nicholson, J., Geller, J., Fisher, W., & Dion, G. (1993). State policies and programs that address the needs of mentally ill mothers in the public sector. Hospital and Community Psychiatry, 44(5),
484-489.
6. Sutker, P. (1981). Drug dependent women. In B. Reed, G. Beschner, & J. Mondanaro (Eds.), Treatment Services for Drug Dependent Women (Vol. 1). Washington, DC: U.S. Government
Printing Office.
7. Rosenbaum, M. (1979). Difficulties in taking care of business: women addicts as mothers. American Journal of Drug and Alcohol Abuse, 6(4), 431-446.
8. Finkelstein, N. (1994). Treatment issues for alcohol- and drugdependent
pregnant and parenting women. Health and Social Work, 19, 7-15.
9. Gomberg, E. (1993). Women and Alcohol: Use and Abuse. The Journal of Nervous and Mental Disease, 181, 211-219.
10. Herman, J. (1992). Trauma and Recovery. NY: Basic Books.
11. Najavits, L., Weiss, R., & Shaw, S. (1997). The link between substance abuse and posttraumatic stress disorder in women: A research review. American Journal on Addictions, 6(4), 273-283.
12. Egeland, B., Jacobvitz, D.,& Sroufe, A. (1988). Breaking the cycle of abuse. Child Development, 59, 1080-1088.
13. Finkelstein, 1994
14. Beckman, L. & Amaro, H. (1986). Personal and social difficulties faced by females and males entering alcoholism treatment. Journal of Studies on Alcohol, 45,135-45.
15. Finkelstein, 1994
16. Chavkin, W. & Kandall, S.R. (1990). Between a “rock” and a hard place: Perinatal drug abuse. Pediatrics, 85, 223-225.
17. Nicholson et al,1993
18. Harmer, A., Sanderson, J., & Mertin, P. (1999). Influence of negative childhood experiences on psychological functioning, social support, and parenting for mothers recovering from addiction. Child Abuse and Neglect, 23(5), 421-33.
19. Grella, 1996
20. Morris, S. & Schinke, S. (1990). Treatment needs and services for mothers with a dual diagnosis: Substance abuse and mental llness. Journal of Offender Counselling Services and Rehabilitation, 15(1), 65-84.
21. Harmer et al., 1999
22. Famularo, R., Barnum, R., & Stone, K. (1986). Court-ordered removal in severe child maltreatment: An association to parental
major affective disorder. Child Abuse and Neglect, 10, 487-492.
23. Hammen, C. (1997). Children of depressed parents: The stress context. In Wolchik, S., Sandler, I. et al., (Eds). Handbook of Children’s Coping: Linking Ttheory and Intervention. Issues in Clinical Child Psychology (pp. 131-157). New York, NY: Plenum
Press.
24. Lyons-Ruth K, Block D. (1996). The disturbed caregiving system: Relations among childhood trauma, maternal caregiving, and infant affect and attachment. Infant Mental Health Journal ,17, 257-275.
25. Famularo, R., Kinscherff, R., & Fenton, R. (1992). Parental substance abuse and the nature of child maltreatment. Child Abuse and Neglect, 16, 475-483.
26. Mallouh, C. (1996). The effects of dual diagnosis on pregnancy and parenting. Journal of Psychoactive Drugs, 28(4), 367-378.
27. Finkelstein, N., Brown, K., & Laham, C. (1981). Alcoholic mothers and guilt: Issues for caregivers. Alcohol Health and Research World., Fall 1991, 45-49.
28. Gabinet, L. (1986). A protocol for assessing competence to parent a newborn. General Hospital Psychiatry, 8(4), 263-272.
29. Nicholson et al., 1993
30. Bavelok, S. (1984). Handbook for the AAPI, Adolescent Parenting Inventory. Eau Claire, WI: Family Development Resources, Inc.
31. Morris & Schinke, 1990
32. Finkelstein et al., 1981
33. Camp, J. & Finkelstein, N. (1995). Fostering Effective Parenting Skills and Healthy Child Development Within Residential Substance Abuse Treatment Settings. Report prepared for Coalition on Addiction, Pregnancy, and Parenting. Boston: Health and Addictions Research, Inc.
34. For a comprehensive review of program design issues see Grella, C. (1997). Services for perinatal women with substance abuse and mental health disorders: The unmet need. Journal of Psychoactive Drugs, 29, 67-78.
35. Finkelstein, N. (1993). Treatment Programming for Alcohol and Drug-Dependent Pregnant Women. International Journal of the Addictions, 28(3). 1275-1309.
The Women, Co-Occurring Disorders and Violence Study is generating knowledge on the development of integrated services approaches for women with co-occurring mental health and substance abuse disorders who also have histories of physical and/or sexual abuse.
This fact sheet is a product of the Women, Co-Occurring Disorders and Violence Coordinating Center which is operated by Policy Research Associates, in partnership with The Better Homes Fund, Community Connections and the Cecil G. Sheps Center for Health Services Research at the
University of North Carolina, Chapel Hill.
The Coordinating Center provides technical assistance to program sites, conducts cross-site process and outcome evaluations, and develops a range of application products from the study sites. This publication was developed by The Better Homes Fund.
The Women, Co-Occurring Disorders and Violence Study is funded by the Substance Abuse and Mental Health Services Administration’s three centers – The Center for Substance Abuse Treatment, The Center for Substance Abuse
Prevention, and The Center for Mental Health Services.
For more information on this Initiative, please contact Policy Research Associates, 262 Delaware Avenue, Delmar, NY, 12054, 518-439-7415, email: wvcc.prainc.com. or visit the study’s web site at www.prainc.com/wcdvs
References
Click Here for ncsacw.samhsa.gov/tutorials/pdf2/ParentingFactSheet.pdf