benzo
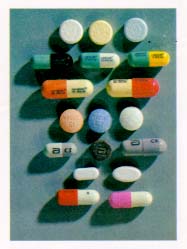 A benzodiazepine (pronounced /ˌbɛnzɵdaɪˈæzɨpiːn/, sometimes colloquially referred to as a “benzo”, and often abbreviated in the literature as a “BZD”) is a psychoactive drug whose core chemical structure is the fusion of a benzene ring and a diazepine ring.
A benzodiazepine (pronounced /ˌbɛnzɵdaɪˈæzɨpiːn/, sometimes colloquially referred to as a “benzo”, and often abbreviated in the literature as a “BZD”) is a psychoactive drug whose core chemical structure is the fusion of a benzene ring and a diazepine ring.
The various benzodiazepines are listed in order of the shortest acting to the longest acting (by the approximate elimination half-life of the drug), however this time may greatly vary between persons.
triazolam (Halcion®) – 2 hours
midazolam (Versed®, Hypnovel®) – 3 hours (1.8-6 hours)
oxazepam (Serax®) – 4-15 hours
chlordiazepoxide (Librium®) – 5-25 hours
alprazolam (Xanax®) – 6-12 hours
temazepam (Restoril®) 8-20 hours
lorazepam (Ativan®) 10-20 hours
bromazepam (Lexotan®) 10-20 hours
estazolam (ProSom®) 10-24 hours
flunitrazepam (Rohypnol®) 18-26 hours. Withdrawn from the market; considered a “date-rape drug”
clonazepam (Klonopin®, Rivotril®) 18-50 hours
quazepam (Doral®) 25-100 hours
clorazepate (Tranxene®) 36-100 hours
medazepam (Nobrium®) 36-150 hours
prazepam (Centrax®) 36-200 hours
diazepam (Valium®) 36-200 hours
flurazepam (Dalmane®) 40-250 hours
The first benzodiazepine, chlordiazepoxide (Librium), was discovered accidentally by Leo Sternbach in 1955, and made available in 1960 by Hoffmann–La Roche, which has also marketed diazepam (Valium) since 1963.
Benzodiazepines are considered to be major drugs of abuse.
Benzodiazepine abuse is mostly limited to individuals who abuse other drugs, i.e. poly-drug abusers. The majority of prescribed users do not abuse their medication. Internationally, benzodiazepines are categorized as Schedule IV controlled drugs by the INCB, apart from flunitrazepam, which is a Schedule III drug under the Convention on Psychotropic Substances.
Some variation in drug scheduling exists in individual countries; for example in the United Kingdom midazolam and temazepam are Schedule III controlled drugs. Benzodiazepine abuse ranges from occasional binges on large doses, to chronic and compulsive drug abuse of high doses.
Benzodiazepines are used recreationally and by problematic drug misusers. Mortality is higher among poly-drug misusers that also use benzodiazepines. Heavy alcohol use also increases mortality among poly-drug users.
Dependence and tolerance, often coupled with dosage escalation, to benzodiazepines can develop rapidly among drug misusers; withdrawal syndrome may appear after as little as three weeks of continuous use. Long-term use has the potential to cause both physical and psychological dependence and severe withdrawal symptoms such as depression, anxiety and panic attacks, and agoraphobia.
Benzodiazepines and in particular temazepam, are sometimes used intravenously, which if done incorrectly or in an unsterile manner, can lead to medical complications including abscesses, cellulitis, thrombophlebitis, arterial puncture, deep vein thrombosis and gangrene.
Sharing syringes and needles for this purpose also brings up the possibility of transmission of hepatitis, HIV and other diseases. Benzodiazepines are also misused intranasally, which may have additional health consequences.
Once benzodiazepine dependence has been established, a clinician usually converts the patient to an equivalent dose of diazepam before beginning a gradual reduction program.
A 1999–2005 Australian police survey of detainees reported preliminary findings that self-reported users of benzodiazepines were less likely than non-user detainees to work full-time and more likely to receive government benefits, use methamphetamine or heroin and be arrested or imprisoned.
Benzodiazepines are sometimes used for criminal purposes; they serve to incapacitate a victim in cases of drug assisted rape or robbery.